2025 Open Enrollment Resources
Open Enrollment is from November 4th – 18th
For questions, please contact HelloFresh Benefits
and Payroll Connect at 877-431-7867
Open Enrollment Resources
2025 Open Enrollment Guide – English
2025 Open Enrollment Guide – Spanish – Coming Soon
Enrollment Instructions and Assistance
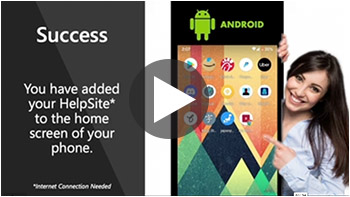
Enrollment Instructions – Desktop & Android & Apple
Benefits and Payroll Connect Service Center
For questions, please contact HelloFresh
Benefits and Payroll Connect at 877-431-7867
Cigna – Medical
Plan Information
Coverage Period: January 1, 2025 to December 31, 2025
Group Number: 3345209
Member Services: 877.501.7990
Member Website: https://www.CIGNA.com
Cigna – Medical
Additional Documents
Preventive Care Flyer – English & Spanish
Virtual Care Flyer – English & Spanish
Personify Wellness Flyer
Personify Wellness Rewards
Pharmacy Flyer – English & Spanish
Pharmacy Formulary – English & Spanish
Behavioral Health Flyer
Cigna One Guide – English & Spanish
Diabetes and Hypertension Support
Musculosketal Program
Spending Accounts
NEW Group Specified Disease Plan
Group Accident Plan
Employee Discounts

Coverage Period: January 1 to December 31
Group Number: 3345209
Member Services: 877.501.7990
Member Website: https://www.CIGNA.com
How to find a Doctor:
Cigna Health Care Provider Directory
Medical Videos, Guides & Links
2024 Medical Documents
2024 Traditional OAP $1,500 Benefit Summary
2024 Traditional OAP $4,000 Benefit Summary
2024 HDHP-HSA $1,600 Benefit Summary
2024 Traditional OAP $1,500 Plan SBC
2024 Traditional OAP $4,000 Plan SBC
2024 HDHP-HSA $1,600 Plan SBC
2024 Traditional OAP $1,500 Plan SPD
2024 Traditional OAP $4,000 Plan SPD
2024 HDHP-HSA $1,600 Plan SPD
2024 Trad $1500 & HDHP-HSA SPC Cert Rider
2024 Traditional OAP $4,000 SBC Cert Rider
CIGNA One Guide Documents
CIGNA Open Access + Documents
My CIGNA Documents
ATTENTION! myCigna Portal is available to members




Use the QRCode above to learn how to register at myCigna.com. (PDF: myCigna Flyer)
Compliance Links
Cigna – Machine Readable Files
This link leads to the machine readable files that are made available in response to the federal Transparency in Coverage Rule and includes negotiated service rates and out-of-network allowed amounts between health plans and healthcare providers. The machine-readable files are formatted to allow researchers, regulators, and application developers to more easily access and analyze data.





Coverage Period: January 1 to December 31
Group Number: 3345209
Member Services: 877.501.7990
Member Website: https://www.CIGNA.com
Rx Videos, Guides & Links
Pharmacy Documents
Pharmacy Welcome Letter
About Cigna 90 Now Letter
National Preferred July 2023 Prescription Drug List – English & Spanish
Formulary Clinical Update January 2024
Formulary Changes January 2024
Patient Assurance Program – English – Spanish
90-Day Prescription Fills Flyer – English – Spanish
Rx Claim Form with Instructions





Coverage Period: January 1 to December 31
Group Number: 3345209
Member Services: 877.501.7990
Member Website: https://www.CIGNA.com
Wellbeing Videos, Guides & Links
Wellbeing Documents
Diabetes and Hypertension Support
Omada Health Program Access
Omada Health Program Details
Healthy Joints and Pain Relief Support
Hinge Health Flyer – English – Spanish
Veteran Support
Veteran Support and Mindfulness Flyer – English
Pregnancy Support
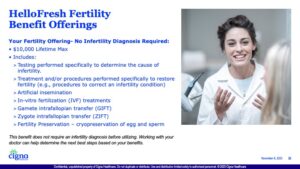
Conception Care Fertility Benefits – English – Spanish
Infertility Benefits – English
Healthy Pregnancy, Healthy Baby Book – English & Spanish
Healthy Pregnancy Rewards – English & Spanish
Breast Pump Order Flyer – English & Spanish
Gender Affirmation Support
My Personal Champion – English & Spanish
There is no charge for MDLive for employees that have the OAP plans.
For those that have the HDHP plan the average per visit charge is between $55 – $125, HOWEVER there is no charge through 12/31/2024!
![]()
![]()
Coverage Period: January 1 to December 31
Schedule Your Appointment: 888.726.3171
Website: MDLive for Cigna
Virtual Care Videos


Use the QRCode above to learn More about your Dental Virtual Care benefit. (Video: Dental Virtual Care)
Dental Virtual Care Documents


Coverage Period: January 1 to December 31
Group Number: 3345209
Member Services: 877.501.7990


Coverage Period: January 1 to December 31
Group Number: 1000278614
Member Services: 800.532.3327
Member Services Fax: 800.726.9982
PIN & Password Assistance: 800.840.7684
Fax Number: 800.726.9982
Website: flores247.com
Mailing Address
Flores & Associates, LLC
PO Box 31397
Charlotte, NC 28231





Coverage Period: January 1 to December 31
Group Number: 3345209
Member Services: 800.244.6224
Website: Cigna.com
ATTENTION!
myCigna Portal is available to members




Use the QRCode above to learn how to register at myCigna.com. (PDF: myCigna Flyer)
How to find a Dentist:
Cigna Health Care Provider Directory
Provider Directory Link
Network = DPPO


Use the QRCode above to learn more about your Cigna Dental PPO Plan. (Video: Cigna DPPO)


Use the QRCode above to learn more about your Dental Preventive Care benefit. (Video: Dental Preventive Care)




Use the QRCode above to learn More about your Dental Virtual Care benefit. (Video: Dental Virtual Care)
Dental Documents


Coverage Period: January 1 to December 31
Group Number: 1029949
Member Services: 866.800.5457
(Mon-Sat, 7:30am-11:00pm EST,
Sun 11:00am-8:00pm EST)
For LASIK: 800.988.4221
Website: EyeMed.com
Vision Documents
FAQs
Additional Documents





Coverage Period: January 1 to December 31
Group Number: 652467
Member Services: 800.421.0344
Claims: 866.868.6737
Unum Portal: Member Portal
Basic Life Documents
(Employer Paid Life)
FAQs
Voluntary Life Documents
2024 Voluntary Life and AD&D Rates
Voluntary Life and AD&D Insurance Plan – English & Spanish
Voluntary Life and AD&D Booklet
Statement of Health – Evidence of Insurability
Portability and Conversion Options
Application for Conversion – Most States | New York | Pennsylvania
Application for Portability – Most States | New York |





Coverage Period: January 1 to December 31
Group Number: 652467
Member Services: 800.421.0344
Claims: 866.868.6737
Unum Portal: Member Portal
Long-Term Documents
Long-Term Buy-up Documents
FAQs





New for 2024: Hospital Insurance and Accident Insurance offered by UNUM.
Coverage Period: January 1 to December 31
Group Number: (Coming Soon)
Member Services: 866.679.3054
8 am – 8 pm EST
Unum Portal: Member Portal
Group Accident Plan Documents
Accident Plan Overview – English & Spanish
Be Well Incentive – English & Spanish
Accident Certificate
Accident Claim Form
Application for Portability – Most States | New York | New Jersey
Group Hospital Plan Documents
Hospital Plan Overview – English & Spanish
Hospital Plan Certificate
Hospital Claim Form
Application for Portability – Most States | New York | New Jersey


Plan Number: 551637
Verification Number: 55163799
Enrollment Services: 888.311.9487
Member Services: 800.584.6001
Rollover Services: 866.865.2660
Participant Website: MyVoya.com
Enrollment Website: VoyaEnroll.com
Retirement Documents
Retirement Enrollment





Member Services: 800.854.1446
Website: UNUM.com/LifeBalance
HelloFresh has partnered with Bright Horizons to support care and education needs for you and your family.


Website: BrightHorizons.com
Phone Number: 877-242-2737
Website Login Information
Employer User Name: hellofresh
Password: hfcares


Member Services: 866.799.2655
Email: [email protected]
You can receive personalized alerts about tests and screenings, check the status of a case in real time, view a snapshot of your benefits package, read healthy tips and articles, hands-free tracking with Apple Health and other fitness devices available to members with Wellness, and Access 24/7 live support to help with healthcare- and insurance-related issues.
Wrap Document
HelloFresh – Protection Against Surprise Billing
Important Notice About Your Prescription Drug Coverage and Medicare
Comprehensive Notice of Privacy Policy and Procedures
Employee Healthcare Plan Notice of Special Enrollment Rights
COBRA General Notice
Notice of Right to Designate Primary Care Provider and of No Obligation for Pre-Authorization for OB/GYN Care
Women’s Health and Cancer Rights Notice
Michelle’s Law Notice
Premium Assistance Under Medicaid and the Children’s Health Insurance Program (CHIP)
Summary Annual Report for Retirement Savings Plan
Summary Annual Report for Health and Wellfare
Health Care Security Ordinance (HCSO)
Medicare Notice
Helpful Terminology
Provider: A clinic, hospital, doctor, lab, health care practitioner, or pharmacy.
Insurer or carrier: The insurance company providing coverage to the policy holder.
Policyholder: The individual or business (“group”) that has entered a contractual relationship with the insurance company.
Insured: The person with the health insurance coverage. For individual health insurance, you may be both the policy holder and the insured.
Premium: The amount of money charged by an insurance company for coverage. The cost of premiums may be determined by several factors, including age, geographic area, number of dependents and tobacco consumption. Policy holders pay these rates annually or in smaller payments over the course of the year, and the amount may change over time. When insurance premiums are not paid, the policy is typically considered void, and companies will not honor claims against it. Self-employed persons may deduct the cost of their individual health insurance premiums from their taxes.
Copayment (Copays): A fixed amount you pay for a covered health care service, usually when you get the service. The amount can vary by the type of covered health care service.
Deductible: The amount you owe for health care services each year before the insurance company begins to pay. For example, if your annual deductible is $1,000, your plan won’t pay anything until you’ve met your $1,000 deductible for covered health care services that are subject to the deductible. The deductible may not apply to all services, such as preventive care services.
Deductibles are useful for keeping the cost of insurance low. The amount varies by plan, with lower deductibles generally associated with higher premiums. They are standard on most types of health coverage.
Coinsurance: Your share of the costs of a covered health care service calculated as a percent (for example, 20 percent) of the allowed amount for the service. You pay coinsurance plus any deductibles you still owe for a covered health service.
Out-of-Pocket Maximum: The most you will be required to pay for your health care during a year, excluding the monthly premium. It protects you from very high medical expenses. After you reach the annual out-of-pocket maximum, your health insurance or plan begins to pay 100 percent of the allowed amount for covered health care services or items for the rest of the year. Copays, deductibles, and coinsurance count towards the out-of-pocket maximum.
Preventive Care: Medical tests and checkups, immunizations, and counseling services used to prevent chronic illness from occurring.
Formulary: A list of prescription drugs covered by the plan. Also called a drug list.
In-Network: A group of doctors, clinics, hospitals, and other healthcare providers that have an agreement with your medical plan provider. You pay a negotiated rate for services when you use in-network providers.
Out-of-Network: Care received from a doctor, hospital or other provider that is not part of the plan agreement. You’ll pay more when you use out-of-network providers since they don’t have a negotiated rate with your plan provider. You may also be billed the difference between what the out-of-network provider charges for services and what the plan provider pays for those services
High Deductible Health Plan (HDHP): This is a type of medical plan that requires the member to reach a deductible prior to having services covered by coinsurance. All expenses paid by the member count toward the deductible and out-of-pocket maximum.
Guaranteed Issue: The amount of coverage that you can receive without having to answer health questions (Evidence of Insurability). The guaranteed issue applies to the voluntary life plan.
Evidence of Insurability: Evidence of Insurability (EOI) is an application with medical questions that you complete in order to be considered for certain types of insurance coverage. Evidence of Insurability applies to the voluntary life and buy-up long-term disability plans.
We welcome your feedback on your HelpSite , please email us at [email protected] | Privacy Policy
© BenefitHelp All Rights Reserved
DISCLAIMER
Every reasonable effort has been made for the information provided to be accurate. It is intended to provide an overview of the coverage’s offered. It is in no way a guarantee or offer of coverage. Each carrier has the ability to underwrite based on its contract. Each carrier’s contract, underwriting, and policies will supersede the information on this page. Please be aware that each carrier may have exclusions or limitations and you must consult your summary plan description and/or policies for details.