My Employee Benefits
Our employees are our greatest resource and we take pride in being able to offer comprehensive and affordable benefits for all of our employees and their families.

To register, FIRST TIME ONLY
Use Company Identifier = Tier1Fire
RETURNING Users Login Above
How to use the System Video
Read about your benefits
12/5 Meeting replay click above
Click on one of the tabs to learn more about that benefit.
Plan starting 1-1-25
![]()
First Primary Care Website
Member / Provider Support: (832) 737-8622
About the FPC Program
Coverage Period:
JAN 1 – DEC 31
Group Number: FPCTF
Medical Claims Administrator For Doctor, Medical, and Rx Support:
Contact Yuzu
Phone: (203) 208-9898
E-mail: [email protected]
Website: www.yuzu.health
Member portal: yuzu.health/signin
Rx Perscription Administrator
First, check Magic Pill using the Magic Pill App
Drexi is the Pharmacy Benefit Manager
www.drexi.com
Member portal: drexi.com/signin
Phone (844) 728-3479 Customer Service
Phone (877) 668-5461 Rx Advocacy
Rx Bin: 018448
PCN: 66202303

Find a Cigna provider: Click here
The new DPC (Direct Primary Care) Plan is through First Primary Care. We are the quarterback to guide you through the healthcare maze.
Before the start of your Plan:
If you have upcoming appointments, have a relationship with a PCP or are on prescription medications and want help understanding how you will continue accessing care, please answer the questions in this document and someone from the FPC team will reach out when they have an answer. Use this link
On or after the effective date of your Plan.
New Member Welcome Kit
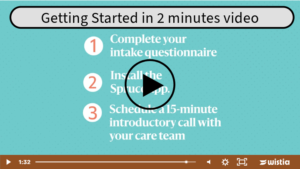
Getting Started One Page Three Easy Steps
(you will receive an e-mail on the 1st day your plan becomes effective)
Medical
SBC – Summary of Benefits & Coverage
Simple One Page Summary – English
About the PFC Program
Labs Included with DPC Membership
Video about the plan – coming soon
Prescription Drugs (Rx)
Magic Plill Program and Drug List – 2024
Get the Magic Pill Phone app for Apple IOS
Additional Information
Medical 2025 Plan Summary

Plan Year: Jan. 1 through Dec. 31 (Enrolled before 8-1)
If enrolled after 8-1 See Ameriflex information below.
Customer Service: 1-866-346-5800
Health Equity Website
Click Here to Log Into Your Account
Health Savings Account Information
HSA Eligible Expenses
Helpful Documents
Flexible Spending Account
Premium Only Plan
FSA Overview
FSA Eligible Expenses
FSA Claim Form
HSA/FSA Options
Health Savings Account (Only Eligible with the HDHP Medical Plan)
Employees may set aside, via payroll on a pre-tax basis, funds to pay the health insurance deductible and
qualified medical expenses, including dental and vision care. An HSA account is only valid with the High
Deductible Medical Plan.
Healthcare: Up to $3,850 for an individual and $7,750 for a family can be set aside to pay for certain
eligible expenses. Individuals 55 and older can save an additional $1,000.
Flexible Savings Account (Only Eligible with the CoPay Medical Plan)
Employees may set aside, via payroll on a pre-tax basis, funds to pay the health insurance deductible and
qualified medical expenses, including dental and vision care.
Healthcare: Up to $3,050 can be set aside to pay for certain eligible expenses. The maximum carryover
for 2022 is $570.
Dependent Care: Up to $5,000 (Individual or Married Filing Jointly) or $2,500 (Married Filing Separately)
can be set aside to pay for certain childcare and dependent care expenses.
Virtual Care Documents
Virtual Care Documents

Plan Year: Jan. 1 through Dec. 31
Group Number: 1154542
Customer Service: 1-800-247-4695
Dental & vision claims
Principal
P.O. Box 10357
Des Moines, IA 50306-0357
Phone: 800-247-4695
Fax: 866-301-1502
Submit claims:
CSD [email protected]
General claims questions:
[email protected]
Helpful Documents

Plan Year: Jan. 1 through Dec. 31
Group Number: 1154542
Customer Service: 1-800-247-4695
Dental & vision claims
Principal
P.O. Box 10357
Des Moines, IA 50306-0357
Phone: 800-247-4695
Fax: 866-301-1502
Submit claims:
CSD [email protected]
General claims questions:
[email protected]
Plan starting 1-1-25
![]()
Group Number: BCN : E6239990
Customer Service: 1-800-325-4368
TTY/TDD: 1-803-798-4040
Helpful Documents
Critical Illness w/Cancer TN Product Info
Summary Page from Benefits Guide
Critical Illness – RATES
Group Critical Illness Certificate Policy
Facts of Critical Illness
Wellness Screening Claim Form
Critical Illness Claim Form
Universal Claim Form
Request for Service Form
Service Guide
Plan starting 1-1-25
![]()
Group Number: BCN : E6239990
Customer Service: 1-800-325-4368
TTY/TDD: 1-803-798-4040
Helpful Documents
Accident Preferred Product Information
Accident Rates – See Benefit Guide
Accidental Death & Dismemberment benefit included
Group Accident Certificate Policy
Change of Beneficiary FAQ
Change of Beneficiary Form
Plan starting 1-1-25
![]()
Group Number: BCN : E6239990
Customer Service: 1-800-325-4368
TTY/TDD: 1-803-798-4040
Plan starting 1-1-25
![]()
Group Number: BCN : E6239990
Customer Service: 1-800-325-4368
TTY/TDD: 1-803-798-4040
Helpful Documents
What’s the difference between term life and whole life?
Group Voluntary Term Life Info – see Benefit Guide
Group Term Life RATES
Group Term Life Certificate Policy
Whole Life Product Info
Chronic Care Accelerated Benefit
Juvenile Chile Whole Life Info
Whole Life RATES
Whole Life Sample Policy
Change of Beneficiary FAQ
Change of Beneficiary Form
Universal Claim Form
Request for Service Form
Service Guide

Voya 401k – Pretax and Roth Plans
Employees may elect to enroll in a 401k plan through Voya Financial. Employees are eligible after 90 days of employment. Employees must be over 21 to enroll. We offer two ways to invest. Pre-tax 401k: Your contributions are not taxed at the time of investment; taxes will be paid at the time of withdrawals. The company matches 1:1 percent up to employee contribution of 3%; then the company matches 0.5:1 percent for employee contribution of 4-5%. The company matches 4% of employee contribution of above 5%. Roth 401k: Your contributions are invested as after-tax investments. No taxes will be paid at the time of withdrawal. The company matches 1:1 percent up to employee contribution of 3%; then the company matches 0.5:1 percent for employee contribution of 4-5%. The company matches 4% of employee contribution of above 5%. Example: Employee contribution (EE) and Employer contribution (ER); EE:ER = 1:1; 2:2; 3:3; 4:3.5; 5:4; 6:4; 7:4… and so on.
Please contact HR with any additional questions about how to enroll electronically. When eligible, HR will send you via email how to enroll in Tier 1 Fire Protection’s 401k plan.
Plan Number: 551637
Verification Number: 55163799
Enrollment Services: 888.311.9487
Member Services: 800.584.6001
Rollover Services: 866.865.2660
Participant Website: MyVoya.com
Enrollment Website: VoyaEnroll.com
Additional Information Coming Soon
Helpful Documents
|
Important legal information about the Health & Welfare benefits available through Tier 1 Fire Protection LLC is posted at: Access Code: 066T3698 To request a free paper copy of the information included on the website, contact the HR department. |
Documents
2024 Safe Harbor Notice
Health Insurance Marketplace Notice
COBRA Notice
HIPAA Privacy Policy
Surprise Billing Notice
CHIP Notice
Wellness Plan Notice
Notice of Special Enrollment Rights
Rx and Medicare Notice
GINA Notice
OBGYN Notice
USERRA Notice
Michelles Law Notice
Womens Health and Cancer Rights Notice
Newborns and Mothers Health Protection Disclosure
4 Benefit Needs Planning Worksheet – This worksheet guides your benefits choices and how they fulfill your financial needs. TIP- Watch the 4 Needs video
Helpful Terminology
Provider: A clinic, hospital, doctor, lab, health care practitioner, or pharmacy.
Insurer or carrier: The insurance company providing coverage to the policy holder.
Policy holder: The individual or business (“group”) that has entered a contractual relationship with the insurance company.
Insured: The person with the health insurance coverage. For individual health insurance, you may be both the policy holder and the insured.
Premium: The amount of money charged by an insurance company for coverage. The cost of premiums may be determined by several factors, including age, geographic area, number of dependents and tobacco consumption. Policy holders pay these rates annually or in smaller payments over the course of the year, and the amount may change over time. When insurance premiums are not paid, the policy is typically considered void, and companies will not honor claims against it. Self-employed persons may deduct the cost of their individual health insurance premiums from their taxes.
Copayment (Copays): A fixed amount you pay for a covered health care service, usually when you get the service. The amount can vary by the type of covered health care service.
Deductible: The amount you owe for health care services each year before the insurance company begins to pay. For example, if your annual deductible is $1,000, your plan won’t pay anything until you’ve met your $1,000 deductible for covered health care services that are subject to the deductible. The deductible may not apply to all services, such as preventive care services.
Deductibles are useful for keeping the cost of insurance low. The amount varies by plan, with lower deductibles generally associated with higher premiums. They are standard on most types of health coverage.
Coinsurance: Your share of the costs of a covered health care service calculated as a percent (for example, 20 percent) of the allowed amount for the service. You pay coinsurance plus any deductibles you still owe for a covered health service.
Out-of-Pocket Maximum: The most you will be required to pay for your health care during a year, excluding the monthly premium. It protects you from very high medical expenses. After you reach the annual out-of-pocket maximum, your health insurance or plan begins to pay 100 percent of the allowed amount for covered health care services or items for the rest of the year. Copays, deductibles, and coinsurance count towards the out-of-pocket maximum.
Preventive Care: Medical tests and checkups, immunizations, and counseling services used to prevent chronic illness from occurring.
We welcome your feedback on your HelpSite , please email us at [email protected] | Privacy Policy
[lmt-post-modified-info]
✟ © BenefitHelp All Rights Reserved
DISCLAIMER
Every reasonable effort has been made for the information provided to be accurate. It is intended to provide an overview of the coverage’s offered. It is in no way a guarantee or offer of coverage. Each carrier has the ability to underwrite based on its contract. Each carrier’s contract, underwriting, and policies will supersede the information on this page. Please be aware that each carrier may have exclusions or limitations and you must consult your summary plan description and/or policies for details.